- Research
- Open access
- Published:
Decoding the key compounds and mechanism of Shashen Maidong decoction in the treatment of lung cancer
BMC Complementary Medicine and Therapies volume 23, Article number: 158 (2023)
Abstract
Background
Lung cancer is a malignant tumour with the fastest increase in morbidity and mortality around the world. The clinical treatments available have significant side effects, thus it is desirable to identify alternative modalities to treat lung cancer. Shashen Maidong decoction (SMD) is a commonly used traditional Chinese medicine (TCM) formula for treating lung cancer in the clinic. While the key functional components (KFC) and the underlying mechanisms of SMD treating lung cancer are still unclear.
Methods
We propose a new integrated pharmacology model, which combines a novel node-importance calculation method and the contribution decision rate (CDR) model, to identify the KFC of SMD and to deduce their mechanisms in the treatment of lung cancer.
Results
The enriched effective Gene Ontology (GO) terms selected from our proposed node importance detection method could cover 97.66% of enriched GO terms of reference targets. After calculating CDR of active components in key functional network, the first 82 components covered 90.25% of the network information, which were defined as KFC. 82 KFC were subjected to functional analysis and experimental validation. 5–40 μM protocatechuic acid, 100–400 μM paeonol or caffeic acid exerted significant inhibitory activity on the proliferation of A549 cells. The results show that KFC play an important therapeutic role in the treatment of lung cancer by targeting Ras, AKT, IKK, Raf1, MEK, and NF-κB in the PI3K-Akt, MAPK, SCLC, and NSCLC signaling pathways active in lung cancer.
Conclusions
This study provides a methodological reference for the optimization and secondary development of TCM formulas. The strategy proposed in this study can be used to identify key compounds in the complex network and provides an operable test range for subsequent experimental verification, which greatly reduces the experimental workload.
Introduction
Lung cancer is the most common primary malignancy and ranks first in the incidence and mortality of malignant tumors in the world. The incidence of lung cancer has reached 11.6% of total cancer cases, and mortality is 18.4% of total cancer deaths [1]. At present, lung cancer treatments mainly include surgery, radiation, and chemotherapy. These treatments can prevent the malignant development of tumor cells and improve survival time. However, most treatments present obvious side effects in clinical use, and can cause serious or general damage to specific or all tissues, including functional damage to the digestive system and urinary system [2]. In addition to the above treatments, some targeted drugs are often used in the clinical treatment of lung cancer, including gefitinib [3], bevacizumab [4], and osimertinib [5], but with these drugs it is difficult to control toxicity and side effects. Thus, it is desirable to improve the treatment for lung cancer.
Many clinical studies have shown that anti-lung cancer treatment combined with Traditional Chinese Medicine (TCM) can reduce the side effects of radiotherapy and chemotherapy, improve therapeutic effects, and reduce complications. Meanwhile, TCM can prolong the life of lung cancer patients and improve their survival quality of life [6]. Currently, some studies have shown that TCM formulas could effectively treat lung cancer. For example, a well-known Yangyinwenyang formula was used to induce lung cancer cell apoptosis in vitro [7]. Jinfukang’s formula could inhibit lung cancer cell proliferation by promoting cell apoptosis [8]. Kangliuzengxiao decoction is successful for the prevention the development of tumors and improving major clinical symptoms [9]. Shashen Maidong Decoction (SMD) can alleviate symptoms of patients and can reduce the inflammatory response [10]. Among these formulas, SMD is widely used in the clinical treatment of lung cancer. As reports, based on the cancer toxicity theory, the application of SMD in treating lung cancer cachexia has definite therapeutic effects and important clinical values [10]. The carcinoembryonic antigen (CEA) and carbohydrate antigen 153 (CA 153) level was significantly reduced in serum of two patient groups [11]. In addition, SMD is proved to have obvious inhibition on the growth of A549 cells. In the result of MTT assay, the growth of A549 cells was inhibited obviously in the SMD-containing serum [12, 13]. A549 cells cultured in the SMD-containing serum showed higher E-cadherin protein expression, lower Snail protein expression (P < 0.05) [12], higher Smad7 protein expression and lower TGF-β1 protein expression [13].
SMD is composed of 7 herbs, Glehnia littoralis (A.Gray) F.Schmidt ex Miq. (G. littoralis, Beishashen, 9 g), Ophiopogon japonicus (Thunb.) Ker Gawl. (O. japonicus, Maidong, 9 g), Polygonatum odoratum (Mill.) Druce (P. odoratum, Yuzhu, 6 g), Trichosanthes kirilowii Maxim. (T. kirilowii, Tianhuafen, 4.5 g), Lablab purpureus subsp. purpureus (L. purpureus, Baibiandou, 4.5 g), Morus alba L. (M. alba, Sangye, 4.5 g), and Glycyrrhiza uralensis Fisch. ex DC. (G. uralensis, Gancao, 3 g). O. japonicus and G. littoralis are the main drugs of SMD, and may be responsible for the therapeutic effects of SMD in lung cancer. Modern pharmacological research indicates that the extract of O. japonicus has an obvious inhibitory effect on the occurrence and development of lung cancer, and it can induce autophagy of A549 lung cancer cells [14]. G. littoralis exerts anticancer activity and induces cycle arrest of A549 cells [15]. In clinical research, SMD combined with hormones or antibiotics is a remarkable treatment for radiation pneumonia [16]. Furthermore, chemotherapy combined with modified SMD has been shown to be highly effective in the cure of mid- and late-stage non-small cell lung cancer (NSCLC) [17]. But there is still a lack reports characterizing key functional components (KFC) and the potential therapeutic mechanism of SMD on lung cancer at a system level.
Due to the “multi-components-multi-targets” of the formula, it is difficult to explore the potential associations among TCM components, target genes, and diseases using traditional experiments. Based on the theory of systems biology, integrated pharmacology can clarify the synergistic mechanism of the components-targets and of the targets-pathogenic network [18]. It is important to study the mechanisms underlying the therapeutic activity of TCM. The “multi-components-multi-targets” characteristic of TCM formulas determine that it could form complex regulation relations between components and targets in the treatment process. Among these complex relationships, some relationships have positive effects on treatment, while others have antagonistic or toxic effects. The aim of formula optimization is a process that finds components with synergistic effects and removes components with antagonistic or toxic effects [19]. Optimization of the formula would be beneficial for the secondary development of TCM.
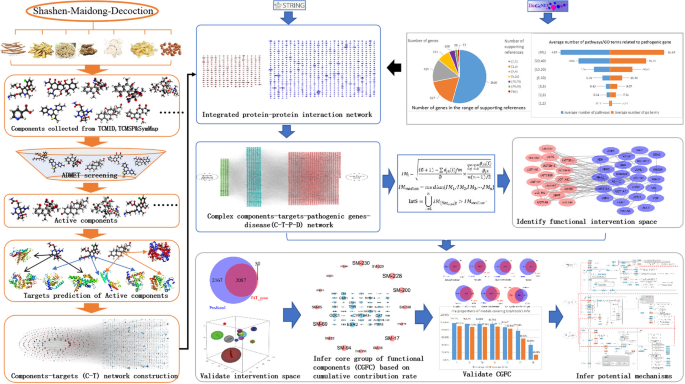
In this study (Fig. 1), the chemicals of SMD were collected from published databases, then the active components were screened from all components based on Lipinski’s rule, oral bioavailability (OB) value, and gastrointestinal (GI) absorption. The targets of active components were predicted using on-line tools, the active components and their targets were used to construct the components-targets (CT) network. Meanwhile, pathogenic genes associated with lung cancer were collected from DisGeNET [20] to construct a network of weighted pathogenic genes. The CT network and the weighted pathogenic gene network were then integrated to construct the CTP network. Finally, a node importance calculation method was designed to select the key functional network and effective proteins. The contribution decision rate (CDR) model was developed to capture KFC. Finally, KFC and their targets were used to infer the potential mechanism of SMD in the treatment of lung cancer.
Materials and methods
Identification of the components of Shashen Maidong decoction and chemical analysis
The component structures of SMD in MOL2 format were downloaded from the Traditional Chinese Medicine Systems Pharmacology Database and Analysis Platform (TCMSP) [21], the Encyclopedia of Traditional Chinese Medicine (ETCM) [22], and Symptom Mapping (SymMap) [23]. The components in different formats were converted into a unified SMILES format by Open Babel 2.4.1 [24]. We searched for experimentally validated high concentrations and biological activities of chemical components of SMD from the literature to obtain a comprehensive list of active components.
Selection of potential active components based on published ADMET models
In general, effective drugs have good absorption, distribution, metabolism, excretion, and toxicity (ADMET) properties. Therefore, in the process of screening possible active components of SMD, we considered some ADMET properties, including Lipinski’s rule [25], GI absorption value [26], and OB [21].
The detailed criteria of Lipinski’s Rule are as follows: there are no more than 5 H-bond donors, less than 10 H-bond acceptors, the molecular weight (MW) is not greater than 500, the calculated Log P is not greater than 5 and the number of rotatable bonds in compounds is less than 10. Ingredients that meet these standards have better drug-like properties.
OB (%F) represents the percentage of oral dose of the chemical components of botanical drugs that are released into the systemic circulation. The chemical components with OB ≥ 30% are well absorbed in human body, so these chemical components were selected for further study.
GI absorption is a pharmacokinetic property, and it is vital to estimate the GI absorption value at each stage of the drug discovery process. GI absorption values of all components in SMD were obtained from SwissADME and chemical components with high GI values were retained for further research.
Predicting the molecular targets of the active components
To obtain the molecular targets of the active components in SMD, we used SwissTargetPrediction [27], HitPick [28], and the Similarity Ensemble Approach (SEA) [29] to predict the potential molecular targets.
Constructing the weighted pathogenic genes network of lung cancer
In the DisGeNET database [20], we identified a total of 27 lung cancer-related international classification of diseases (ICD, version 10) codes by querying “lung cancer” as the key word. We then used these classification IDs to query related genes; a total of 2973 pathogenic genes were obtained.
Definition of protein–protein interaction data
We submitted 2973 pathogenic genes and 1221 predicted targets of active components to the STRING [30] database and chose “Homo sapiens” as the species parameter to obtain the protein–protein interaction (PPI) network.
Construction of component-target network
All SMD chemicals collected in the database were screened with ADMET to obtain active components, and the targets of these active components were predicted by Hitpick, SwissTargetPrediction, and SEA. Active components and their predicted targets were used to construct components-targets (CT) network using Cytoscape [31].
Screening of key functional networks
We constructed a four-layer component-target-gene-disease network by combining CT, PPI network, and pathogenic gene network, and we determined and verified the key component-target-pathogenic gene associations in the network with our newly designed node-importance calculation method. The detailed algorithm was described in the Supporting information.
Prediction of key functional components
The Contribution Decision Rate (CDR) model, which was employed and modified based on knapsack algorithm, was used to determine the KFC in the network: Assuming there is a function that can solve the total value with two dependent variables n and C, the detailed algorithm was described in the Supporting information.
GO and KEGG analysis
R package clusterProfiler [32] was used to perform the Kyoto Encyclopedia of Genes and Genomes (KEGG) [33,34,35] and Gene Ontology (GO) enrichment analysis, and P-value < 0.05 was set as significant level. After that, we used ggplot2 [36] to create the graph of enrichment results. Then, some specific and enriched pathways were merged and visualized to speculate on the potential mechanism of SMD on lung cancer.
Cell culture and treatment
Human lung cancer A549 cells were obtained from GuangZhou Jennio Biotech Co., Ltd. Fetal bovine serum (FBS) and Dulbecco’s modified Eagle’s medium (DMEM) were purchased from Gibco (Grand Island, USA). A549 cells were cultured in DMEM, containing 10% FBS, 100 units/mL of penicillin, and 100 μg/mL of streptomycin at 37℃ under 5% CO2. Protocatechuic acid (≥ 99.5% purity by HPLC), paeonol (≥ 99% purity by HPLC), and caffeic acid (≥ 98% purity by HPLC), which purchased form Jiangsu Yongjian Pharmaceutical Technology Co.,Ltd, were dissolved in DMSO. When the cells reached 80% confluence, they were treated with various concentrations of protocatechuic acid (1, 5, 10, 20, 40 μM), paeonol (25, 50, 100, 200, 400 μM) or caffeic acid (25, 50, 100, 200, 400 μM) for 24 h, respectively. The control group was not treated with drug components.
The concentration of our experimental components was determined referring to public reports. As reported, 80 or 100 μg/mL Paeonol caused a significant effect on cell viability of A549 cells compared to 0 μg/mL Paeonol [37, 38]. Caffeic acid with a concentration higher than 100 μM has significant cytotoxic effect on A549 cells [39]. Protocatechuic acid at 2–8 micromol/L significantly inhibited A549 cell adhesion (P < 0.05) [40].
Cell viability assay
A549 cells (1 × 105 cells/well) were planted in 96-well plates. After a 24-h culture, the cells were treated with different concentrations of protocatechuic acid (1, 5, 10, 20, 40 μM), paeonol (25, 50, 100, 200, 400 μM), or caffeic acid (25, 50, 100, 200, 400 μM) for 24 h, respectively. Subsequently, each well was added with 10 μL of MTT solution (5 mg/ml). After 4 h, the supernatant was removed and 100 μL of DMSO was supplied into each well to dissolve the MTT formazan product. The absorbance was measured at 570 nm using the Infinite M200 PRO plate reader (Tecan, Switzerland).
Results
Collection of chemical components and screening of active components in SMD
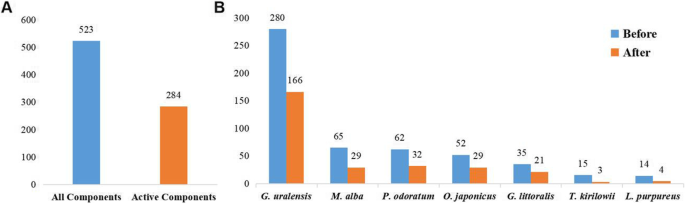
A total of 523 types of chemical components of SMD were retrieved from TCMSP, ETCM, and SymMap databases (Additional Table 1). Among these components, some had higher concentration than expected in SMD by UPLC-MS/MS method (Table 1) [41], such as rutin, liquiritin, psoralen, xanthotoxin, bergapten, monoammonium glycyrhizinate, ophiopogonin D, methylophiopogonanone A, and methylophiopogonanone B. Previous reports confirmed that high-concentration components of SMD may play important roles in the treatment of lung cancer. By combining the experimental validated high-concentration components (Table 1) [41], and ADMET model predicted components, 284 active components were figured out for subsequent analysis (Additional Table 2, Fig. 2).
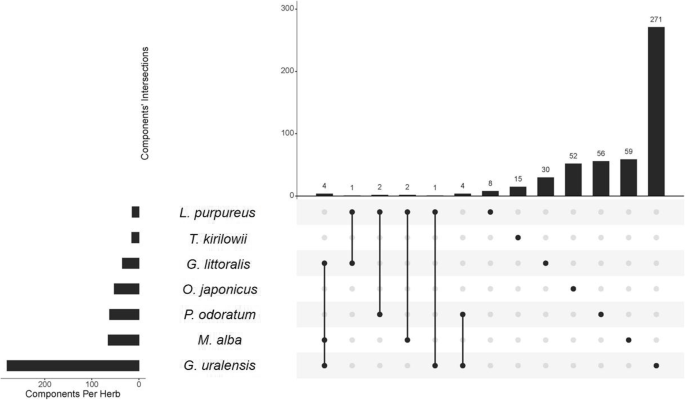
Among all active components, 14 components shared two or multiple herbs in SMD (Fig. 3), quercetin, isoquercitrin, rutin, scopoletol, glucuronic acid, 2-pentylfuran, beta-carotene, gynesine, arachic acid, 2-heptanone, linoleic acid, palmitic acid, oleic acid, and octadiene, have been shown to have clear anticancer effects. For example, quercetin has definite anticancer activity and can inhibit a variety of carcinogenic signaling pathways [42]. Rutin promotes the apoptosis of TNF-α-induced A549 human lung cancer cells [43]. Scopoletol can play an anticancer role by triggering apoptosis, blocking the cell cycle, inhibiting cell invasion, and regulating the PI3K/AKT signaling pathway [44]. Quercetin, isoquercitrin, rutin, and scopoletol are also present in G. littoralis, M. alba and G. uralensis, which may be of great importance in the therapeutic mechanism of SMD on lung cancer. These results indicate that shared components may play important therapeutic roles in lung cancer.
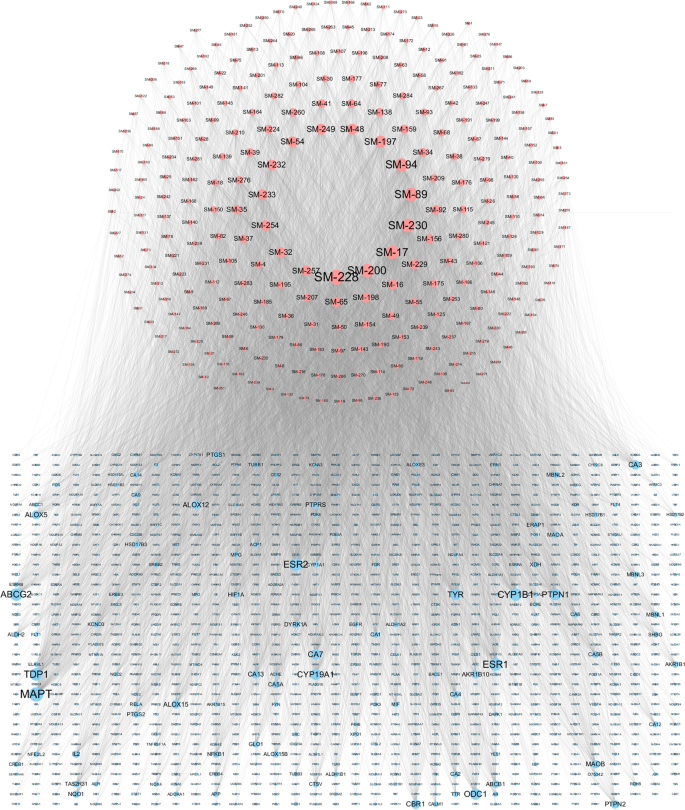
Predicting targets of active components in SMD
The 1221 targets of 284 active components were predicted by SwissTargetPrediction, HITPICK, and SEA (Additional Table 3). The active components and their targets were used to construct the CT network. This network contains 1505 nodes and 11,505 interactions (Fig. 4). We analyzed the degree of each component and each target in this network and found that the average degree of the components was 40.51 and the average degree of the targets was 9.42. Ten components with the highest degree were vanillic acid, ferulic acid, dibenzoylmethane, butyl benzoate, lauric acid, nicotinic acid, dibutyl phthalate, salicylic acid, eugenol, n-cis-feruloyltyramine. Most have been reported to be associated with cancer therapy, vanillic acid has antioxidant activity in scavenging free radicals, and thus, it has an effective preventive effect on lung cancer [45]. Lauric acid can be used as a carrier of targeted drugs due to its specific accumulation in lung cancer tissues [46]. The ten targets with the highest degree of the components were MAPT, ESR1, TDP1, ESR2, CYP1B1, ABCG2, ODC1, PTPN1, CYP19A1, and TYR. Most of these genes are reported to be related to the pathogenesis of lung cancer. MAPT has been shown to induce lung cancer cells to gain taxol resistance by activating the PI3K/Akt signaling pathway [47]. ESR1 is a central gene of lung cancer and promotes the occurrence of lung cancer by regulating the p53 signaling pathway and the cell surface receptor signaling pathway [48]. Overexpression of TDP1 is closely related to tumorigenesis, and is a crucial target for tumor treatment, the TDP1 inhibitor can significantly increase the antitumor effect of drugs [49]. These analyses demonstrate that one component can regulate multiple targets and in turn, one target is regulated by multiple components, which reflects the characteristics of the “multicomponents-multitargets” theory in treating complex diseases of TCM.
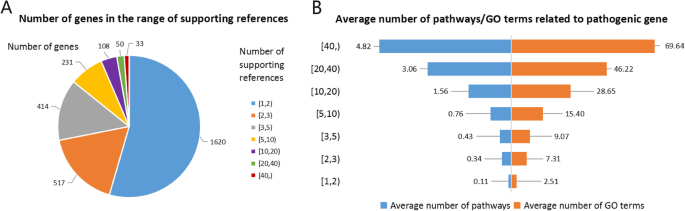
Construction of the pathogenic genes weighted network
The pathogenic gene data set was retrieved and downloaded from the DisGeNET database and 2973 pathogenic genes with the number of supporting publications greater than or equal to the mean value were retained (Additional Table 4). The number of supporting publications reflects the correlation of genes associated with lung cancer. A higher number of supporting publications suggests that genes have more associations with lung cancer. After counting the number of supporting publications for 2973 pathogenic genes (Fig. 5A), we found that more than half of these pathogenic genes have only one supporting reference and 33 pathogenic genes with more than 40 supporting references. The top ten genes with the highest number of supporting publications are EGFR, TP53, KRAS, ALK, GSTM1, CDKN2A, CYP1A1, ERBB2, BCL2, and MET. The epidermal growth factor receptor (EGFR) is a transmembrane glycoprotein of the ErbB family of tyrosine kinase receptors, and activated mutations of EGFR are a remarkable feature of lung cancer [50]. EGFR-activating mutations are highly sensitive to tyrosine kinase inhibitor gefitinib, so gefitinib is commonly used in clinical targeted treatment of NSCLC [51]. TP53-induced glycolytic phosphatase (TIGAR) is a key regulator of glycolysis and apoptosis, which can protect cells from oxidative stress-induced apoptosis and provide the necessary conditions for the survival of cancer cells [52]. Mutations exist widely in many types of lung cancer [53, 54]. KRAS is a potential oncogene and has been reported to have a high mutation rate, which makes cancer cells escape apoptosis-induced cell death [55]. The rearrangement of anaplastic lymphoma kinase (ALK) plays an important role in promoting the occurrence and development of lung cancer [56], thus it becomes an important clinical targeted treatment of ALK-positive NSCLC [57]. To explore whether it is reliable to measure the importance of gene function by the number of relevant supporting publications, we constructed a KEGG and GO analysis of pathogenic genes of lung cancer (Fig. 5B). The results showed that there is a positive correlation between supporting publications and the functional pathways involved by these genes, as well as GO terms. Genes with more supporting publications are associated with a highest number of pathways involved.
Key functional network selection and validation
In formulas that treat complex diseases, some components play major therapeutic roles, some play auxiliary roles, and others play antagonistic roles. The group of components with major therapeutic roles is usually considered KFC. The KFC and their targets form key functional network, embedded within the complex CT network. How to detect the key functional network and KFC is the basis for optimizing TCM formulations. Additionally, the process of drug treatment of diseases is a continuous process of drug interventions through protein–protein interactions. Based on this information, we integrated the CT network and pathogenic gene weighted network to construct the comprehensive CTP network (Additional Fig. 1). Then we designed a new node importance calculation method to capture the key functional network. The nodes larger than the median important values of all nodes in the network were retained, and these nodes and their interactions were defined as the key functional network.
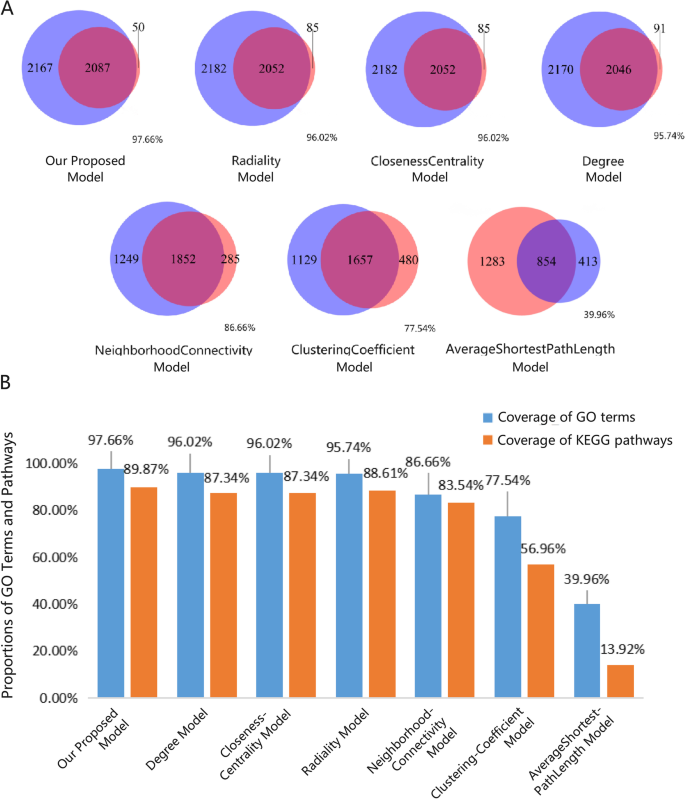
To test the reliability of the node importance calculation method, we first performed GO enrichment analysis on targeted genes and pathogenic genes of lung cancer and considered the intersection of GO terms as the effective GO terms to serve as a reference for further comparison. Comparing our proposed node importance detection method with the other traditional methods (Fig. 6A), such as Radiality, Closeness to center, Degree, Neighborhood Connectivity Clustering coefficient and Average Shortest Path length, we found that our method covered up to 97.66% of effective GO terms, which is higher than Radiality 96.02%, Degree 95.74%, Neighborhood Connectivity 86.66%, and the Clustering Coefficient 77.54%. Figure 6B shows that our model also covered the most pathways, thus it indicated that the key functional network detection model we designed could retain the key intervention information.
Validation of key functional networks. A The Venn diagrams display the number of elements of the seven models that overlap with effective GO terms. The red cycle represents the effective GO terms, and the blue cycle represents the GO terms predicted by different models. B Comparison of our proposed models with other traditional models on the coverage of enriched GO terms and pathways
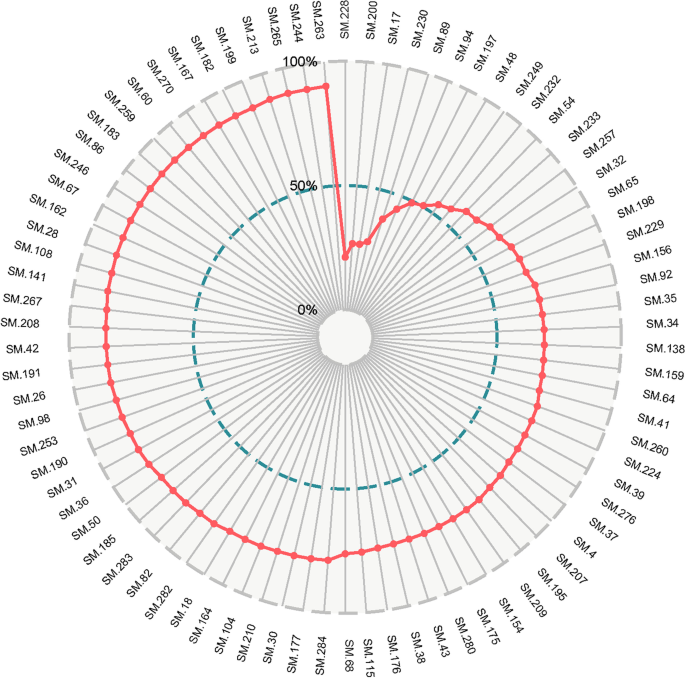
Find key functional components
After extracting the key functional network, we used the CDR model to deduce which components could retain the key functional network information to the maximum extent. Finally, we obtained 82 components that defined the KFC (Additional Table 5, Fig. 7). In the KFC, the CDR of the first 8 components reached 50% target coverage, and the 82 components reached 90% target coverage. Among these components, vanillic acid has been reported to have antioxidant activity in scavenging free radicals and had a significant and effective preventative role in B(a)P-induced lung cancer [45, 46]. Lauric acid is a good carrier of targeted drugs for lung cancer [46] and can also inhibit the expression of carcinogenic miRNA and significantly up-regulate the expression of some cancer-inhibiting miRNA in KB cells and HepG2 cells [58]. Salicylic acid can maintain the stability of the genome and plays a key role in reducing the risk of cancer. These findings indicate that the lack of salicylic acid will lead to the delay of DNA excision and repair mechanisms, the accumulation of single-strand and double-strand breaks, cell cycle arrest, damage from apoptosis, and will increase the susceptibility to cancer development [59].
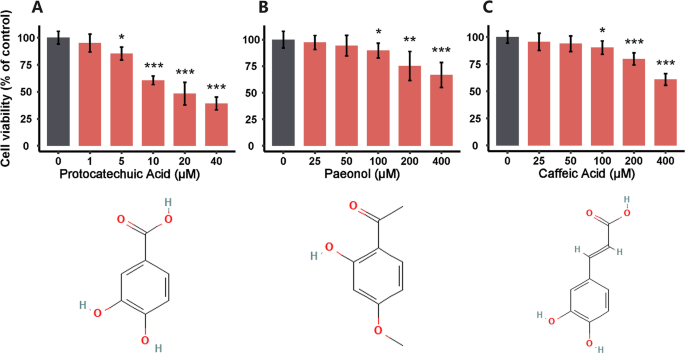
Effects of key functional components on the viability of A549 cells
Simple random sampling is a method of probability sampling based on chance events, and it can mitigate selection bias [60]. It’s the incorporation of randomization that provides unpredictability in treatment assignments. Based on this selective strategy, protocatechuic acid (SM-32), paeonol (SM-257), and caffeic acid (SM-229) in 82 KFC were selected to determine the effects on the viability of A549 cells using the MTT assay. Protocatechuic acid (SM-32) originates from G. uralensis. Paeonol (SM-257) originates from M. alba. Caffeic acid (SM-229) originates from G. littoralis. After 24 h of incubation, the cell viabilities of A549 cells were 95.07 ± 8.30%, 85.31 ± 6.08%, 60.65 ± 4.01%, 48.25 ± 10.39%, and 39.12 ± 5.88% after exposure to protocatechuic acid at concentrations of 1, 5, 10, 20, and 40 μM, respectively (Fig. 8A). After exposure to paeonol at concentrations of 25, 50, 100, 200 and 400 μM, the cell viability was 97.34 ± 6.58%, 94.33 ± 9.72%, 89.77 ± 6.94%, 75.19 ± 13.70% and 66.79 ± 11.76% (Fig. 8B). When cells were treated with 25, 50, 100, 200, and 400 μM caffeic acid, the cell viabilities were 95.60 ± 7.97%, 93.90 ± 7.26%, 90.27 ± 6.18%, 79.91 ± 5.54%, and 60.89 ± 5.39% (Fig. 8C). The results show that 5–40 μM protocatechuic acid, 100–400 μM paeonol or caffeic acid exerted significant inhibitory activity on the proliferation of A549 cells.
Possible therapeutic mechanism
ClusterProfiler was used to perform the functional enrichment analysis of the KFC targeted genes, we obtained pathways with a P-value < 0.05. Among these pathways, the small lung cancer and NSCLC pathways are highly correlated with the pathogenesis of lung cancer. Increasing evidence confirms that the downstream gene regulation of the PI3K/Akt signaling pathway (hsa04151) can be changed by targeting the GPCR receptor family through PI3K and Akt. Furthermore, activation of the PI3K/Akt signaling pathway can inhibit apoptosis, promote gene transcription, and cell proliferation, accelerate the cell cycle process, and promote angiogenesis by regulating various downstream activating factors [61,62,63]. The MAPK signaling pathway (hsa04010) also proved to be vital to the occurrence and development of tumor, and activation of the MAPK signaling pathway may lead to increased proliferation, migration, and invasion of tumor cells [64].
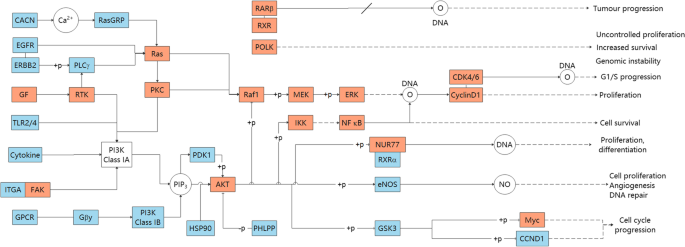
To further explore the synergistic effects of KFC targets in different pathways, we combined the enrichment pathways as a comprehensive pathway. The comprehensive pathway included small lung cancer (hsa05222), NSCLC (hsa05223), the PI3K/Akt signaling pathway (hsa04151), and the MAPK signaling pathway (hsa04010) (Fig. 9, Additional Fig. 2). In the combined pathways, some genes products sharing multiple pathways are named as cross-talk gene products, and main cascade targeting module merged with CDR-predicted comprehensive pathways. Some cross-talk gene products appear intermediately in merged pathways, including Ras, PKC, Raf1, MEK, ERK, CDK4/6, CyclinD1, AKT, IKK, NF-κB, and NUR77. In this module, Ras and AKT frequently regulates downstream receptors, which were also predicted as cross-talk gene products, such as Raf1, MEK, IKK, NF-κB, and so on. The downstream receptors of cross-talk gene products were reported relevant to proliferation and cell survival in other pathways. Myc and POLK, which have indirect effects on increased survival and cell cycle progression, are still worthy of attention. With the prediction of CDR model and the analysis of merged pathways, KFC could act on these targets and deprive indispensable conditions for the proliferation and long-term survival of cancer cells. In this way, therapeutic mechanism could be achieved possibly.
Discussion
Lung cancer is the most common primary malignancy and ranks first in the incidence and mortality of malignant tumors in the world [1]. Lung cancer treatments in clinical usually present obvious side effects in clinical use, and can cause serious or general damage to specific or all tissues [2]. Many clinical studies have shown that anti-lung cancer treatment combined with TCM can reduce the side effects of radiotherapy and chemotherapy, improve therapeutic effects, and reduce complications. Meanwhile, TCM can prolong the life of lung cancer patients and improve their survival quality of life [6]. For example, SMD can alleviate symptoms of patients and can reduce the inflammatory response [10], which is widely used in the clinical treatment of lung cancer. Thus, the potential molecular mechanism of SMD in treating lung cancer was studied based on integrated network pharmacology strategy.
In this study, we designed an integrated network pharmacology strategy to explore the KFC of SMD in the treatment of lung cancer and analyze the possible mechanisms. Herbal components were obtained from TCMSP [21], ETCM [22], and SymMap [23], then potential active components were selected by ADMET properties. The targets of these active components were predicted by Hitpick [28], SwissTargetPrediction [27], and SEA [29], then the CT network was constructed. Pathogenic gene data set was downloaded from the DisGeNET. PPI data of pathogenic genes and predicted targets was obtained from STRING [30] database. Thus, a four-layer component-target-gene-disease network by combining CT, PPI network, and pathogenic gene network, was constructed. With our newly designed node-importance calculation method, key functional network was extracted. Based on knapsack algorithm, KFC were sought out to deduce the maximum target coverage of the key functional network. The accuracy and reliability of the KFC selective method was confirmed further with functional enrichment analysis and in vitro experiments.
Based on integrated network pharmacology strategy, the model designed to explore the KFC of SMD has two measurable advantages. The first is that a novel node-importance calculation model was designed to the figure out key functional networks and validate the coverage rate of key functional networks at functional level. The influence and control of a node to others have been taken into account by the node-importance calculation model, as well as the probability of a node connected to others. The results suggest that the node-importance calculation model we proposed can retain the intervention information to the greatest extent. The second advantage is that we develop the CDR model to capture the KFC in key functional networks. Compared with the traditional pharmacology method based on one-way target speculation mechanisms, the main innovation of our model is that it can provide a methodological reference for the development of integrated pharmacology by considering the spread of the intervention effect from targets to pathogenic genes.
With the prediction of CDR model and the analysis of merged pathways, cross-talk gene products were found, and main cascade targeting module merged with CDR-predicted signalling pathways was visualized clearly. Some cross-talk gene products appear intermediately in merged pathway. Among them, Ras and AKT frequently regulates downstream receptors and other cross-talk gene products, affecting proliferation and cell survival in other pathways. Other cross-talk gene products are still worthy of attention, such as Myc and POLK, despite indirect effects on increased survival and cell cycle progression as reported. After computational analysis and in vitro experiments, KFC could act on these cross-talk gene products to treat lung cancer, and possible therapeutic mechanism could be decoded.
Compared with the traditional pharmacology method based on one-way target speculation mechanisms, the main innovation of our model is that it can provide a methodological reference for the development of integrated pharmacology by considering the spread of the intervention effect from targets to pathogenic genes.
However, it still exists two limitations in our study. First, concentrations of herbal components, that could measure the effects of drug intervention network more exactly, are ignored in our network pharmacological analysis. Second, in order to validate the reliability of our approach, more KFC should be selected to determine the effect of viability of A549 cells or in vivo experiments.
Conclusions
In conclusion, the molecular mechanism of SMD treatment of lung cancer was revealed by integrated network pharmacology model and experimental validation. The strategy proposed in this study can be used to identify key compounds in the complex network and provides an operable test range for subsequent experimental verification, which greatly reduces the experimental workload. In follow-up studies, in vitro and in vivo animal studies can be designed based on the predicted KFC.
Availability of data and materials
All data included in this study are available upon request by contact with the corresponding author. Human data in this study was obtained from public database DisGeNET (https://www.disgenet.org/).
Abbreviations
- ADMET:
-
Absorption, Distribution, Metabolism, Excretion, and Toxicity
- CDR:
-
Contribution Decision Rate
- CI:
-
Contribution Index
- CTP:
-
Components-Targets-Pathogenetic genes
- DL:
-
Drug-Likeness
- DMEM:
-
Dulbecco’s Modified Eagle’s Medium
- FBS:
-
Fetal Bovine Serum
- GO:
-
Gene Ontology
- G. littoralis :
-
Glehnia littoralis (A.Gray) F.Schmidt ex Miq.
- G. uralensis :
-
Glycyrrhiza uralensis Fisch. ex DC.
- ICD:
-
International Classification of Diseases
- KFC:
-
Key Functional Components
- KEGG:
-
Kyoto Encyclopedia of Genes and Genomes
- L. purpureus :
-
Lablab purpureus Subsp. purpureus
- M. alba :
-
Morus alba L.
- NSCLC:
-
Non-Small Cell Lung Cancer
- O. japonicus :
-
Ophiopogon japonicus (Thunb.) Ker Gawl.
- OB:
-
Oral Bioavailability
- P. odoratum :
-
Polygonatum odoratum (Mill.) Druce
- PPI:
-
Protein–Protein Interactions
- SMD:
-
Shashen Maidong Decoction
- SEA:
-
Similarity Ensemble Approach
- SymMap:
-
Symptom Mapping
- TCM:
-
Traditional Chinese Medicine
- TCMSP:
-
Traditional Chinese Medicine Systems Pharmacology Database and Analysis Platform
- T. kirilowii :
-
Trichosanthes kirilowii Maxim
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Ortiz-Cuaran S, Scheffler M, Plenker D, et al. Heterogeneous mechanisms of primary and acquired resistance to third-generation EGFR inhibitors. Clin Cancer Res. 2016;22(19):4837–47.
Lin YT, Chen JS, Liao WY, et al. Clinical outcomes and secondary epidermal growth factor receptor (EGFR) T790M mutation among first-line gefitinib, erlotinib and afatinib-treated non-small cell lung cancer patients with activating EGFR mutations. Int J Cancer. 2019;144(11):2887–96.
Cheng G, Zhang L. Adverse events related to bevacizumab and the management principles in non-small cell lung cancer. Zhongguo Fei Ai Za Zhi. 2010;13(6):563–7.
Zhao Z, Ni Y, Li L, Xin T. Acquired drug resistance mechanism of osimertinib in the targeted therapy of non-small cell lung cancer. Zhongguo Fei Ai Za Zhi. 2020;23(4):274–81.
Su XL, Wang JW, Che H, et al. Clinical application and mechanism of traditional Chinese medicine in treatment of lung cancer. Chin Med J (Engl). 2020;133(24):2987–97.
Zhao B, Hui X, Jiao L, et al. A TCM formula YYWY inhibits tumor growth in non-small cell lung cancer and enhances immune-response through facilitating the maturation of dendritic cells. Front Pharmacol. 2020;11:798.
Zheng X, Wang W, Wang G, Liu S. Could Jinfukang alleviate the chemotherapy-related adverse effects in non-small cell lung cancer patients?: A protocol for a double-blind, randomized controlled trial. Medicine (Baltimore). 2021;100(28):e25002.
Xu ZY, Jin CJ, Zhou CC, et al. Treatment of advanced non-small-cell lung cancer with Chinese herbal medicine by stages combined with chemotherapy. J Cancer Res Clin Oncol. 2011;137(7):1117–22.
He M, Luo Y, Chen L, et al. Shashen maidong decoction: the effect of TNF-alpha and IL-6 on lung cancer cachexia based on cancer toxicity theory. Am J Transl Res. 2021;13(6):6752–8.
Huang QH, Liang YJ, Chen N, Du XT. Effect of Shashen Maidong decoction on tumor marker levels in patients with non-small cell lung cancer. Mod Med Health Res Electron J. 2021;5(12):87–9.
Wang Y, Yang SY, Pan YN, et al. lnfluences of Shashen Maidong decoction-containing serum combined with cisplatin on expressions of E-cadherin and snail in lung adenocarcinoma A549 cells. Chin Arch Tradit Chin Med. 2021;39(08):62–5.
Xu WW, Liu CY. Effect of Shashen Maidong decoction combined with cisplatin on proliferation of lung cancer cell line A549 and expressions of Smad7 and TGF-β1 protein. Liaoning J Tradit Chin Med. 2020;47(05):144–7.
Chen J, Yuan J, Zhou L, et al. Regulation of different components from ophiopogon japonicus on autophagy in human lung adenocarcinoma A549Cells through PI3K/Akt/mTOR signaling pathway. Biomed Pharmacother. 2017;87:118–26.
Wu J, Gao W, Song Z, et al. Anticancer activity of polysaccharide from Glehnia littoralis on human lung cancer cell line A549. Int J Biol Macromol. 2018;106:464–72.
Li S, Zhou X, Xiong H. Clinical study of Shashenmaidong decoction in the treatment of clinical study of Shashenmaidong decoction in the treatment of clinical study of Shashenmaidong decoction in the treatment of clinical study of Shashenmaidong decoction in the treatment of radiation pneumonitis. Acta Chin Med. 2015;30(03):328–9.
Liu M, Wu YL, Zeng R. Observation on the effect of Jiajian Shashen Maidong decoction combined with chemotherapy in the treatment of non-small cell lung cancer. Chin J Clin Rational Drug Use. 2020;13(11):53–4.
Wang KX, Gao Y, Lu C, et al. Uncovering the complexity mechanism of different formulas treatment for rheumatoid arthritis based on a novel network pharmacology model. Front Pharmacol. 2020;11:1035.
Yang L, Fan L, Wang K, et al. Analysis of molecular mechanism of erxian decoction in treating osteoporosis based on formula optimization model. Oxid Med Cell Longev. 2021;2021:6641838.
Pinero J, Ramirez-Anguita JM, Sauch-Pitarch J, et al. The DisGeNET knowledge platform for disease genomics: 2019 update. Nucleic Acids Res. 2020;48(D1):D845–55.
Ru J, Li P, Wang J, et al. TCMSP: a database of systems pharmacology for drug discovery from herbal medicines. J Cheminform. 2014;6:13.
Xu HY, Zhang YQ, Liu ZM, et al. ETCM: an encyclopaedia of traditional Chinese medicine. Nucleic Acids Res. 2019;47(D1):D976–82.
Wu Y, Zhang F, Yang K, et al. SymMap: an integrative database of traditional Chinese medicine enhanced by symptom mapping. Nucleic Acids Res. 2019;47(D1):D1110–7.
O’Boyle NM, Banck M, James CA, Morley C, Vandermeersch T, Hutchison GR. Open Babel: an open chemical toolbox. J Cheminform. 2011;3:33.
Benet LZ, Hosey CM, Ursu O, Oprea TI. BDDCS, the rule of 5 and drugability. Adv Drug Deliv Rev. 2016;101:89–98.
Daina A, Michielin O, Zoete V. SwissADME: a free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci Rep. 2017;7:42717.
Gfeller D, Grosdidier A, Wirth M, Daina A, Michielin O, Zoete V. SwissTargetPrediction: a web server for target prediction of bioactive small molecules. Nucleic Acids Res. 2014;42(Web Server issue):W32–8.
Liu X, Vogt I, Haque T, Campillos M. HitPick: a web server for hit identification and target prediction of chemical screenings. Bioinformatics. 2013;29(15):1910–2.
Keiser MJ, Roth BL, Armbruster BN, Ernsberger P, Irwin JJ, Shoichet BK. Relating protein pharmacology by ligand chemistry. Nat Biotechnol. 2007;25(2):197–206.
Szklarczyk D, Gable AL, Lyon D, et al. STRING v11: protein-protein association networks with increased coverage, supporting functional discovery in genome-wide experimental datasets. Nucleic Acids Res. 2019;47(D1):D607–13.
Shannon P, Markiel A, Ozier O, et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13(11):2498–504.
Yu G, Wang LG, Han Y, He QY. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS. 2012;16(5):284–7.
Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28(1):27–30.
Kanehisa M. Toward understanding the origin and evolution of cellular organisms. Protein Sci. 2019;28(11):1947–51.
Kanehisa M, Furumichi M, Sato Y, Kawashima M, Ishiguro-Watanabe M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 2023;51(D1):D587–92.
Wickham H. ggplot2: Elegant Graphics for Data Analysis. New York: Springer-Verlag; 2016.
Lv J, Zhu S, Chen H, et al. Paeonol inhibits human lung cancer cell viability and metastasis in vitro via miR-126-5p/ZEB2 axis. Drug Dev Res. 2022;83(2):432–46. https://doi.org/10.1002/ddr.21873.
Zhang L, Chen WX, Li LL, et al. Paeonol suppresses proliferation and motility of non-small-cell lung cancer cells by disrupting STAT3/NF-kappaB signaling. Front Pharmacol. 2020;11:572616.
Lin CL, Chen RF, Chen JY, et al. Protective effect of caffeic acid on paclitaxel induced anti-proliferation and apoptosis of lung cancer cells involves NF-kappaB pathway. Int J Mol Sci. 2012;13(5):6236–45.
Yin MC, Lin CC, Wu HC, Tsao SM, Hsu CK. Apoptotic effects of protocatechuic acid in human breast, lung, liver, cervix, and prostate cancer cells: potential mechanisms of action. J Agric Food Chem. 2009;57(14):6468–73.
Sun Y. Chemical composition analysis and pharmacokinetic study of the Shasheng Maidong decoction. PhD thesis. Hebei Medical University; 2016.
Khan F, Niaz K, Maqbool F, et al. Molecular targets underlying the anticancer effects of quercetin: an update. Nutrients. 2016;8(9):529.
Wu F, Chen J, Fan LM, et al. Analysis of the effect of rutin on GSK-3beta and TNF-alpha expression in lung cancer. Exp Ther Med. 2017;14(1):127–30.
Tian Q, Wang L, Sun X, Zeng F, Pan Q, Xue M. Scopoletin exerts anticancer effects on human cervical cancer cell lines by triggering apoptosis, cell cycle arrest, inhibition of cell invasion and PI3K/AKT signalling pathway. J BUON. 2019;24(3):997–1002.
Velli SK, Sundaram J, Murugan M, Balaraman G, Thiruvengadam D. Protective effect of vanillic acid against benzo(a)pyrene induced lung cancer in Swiss albino mice. J Biochem Mol Toxicol. 2019;33(10):e22382.
Reczynska K, Marchwica P, Khanal D, et al. Stimuli-sensitive fatty acid-based microparticles for the treatment of lung cancer. Mater Sci Eng C Mater Biol Appl. 2020;111:110801.
Cai Y, Jia R, Xiong H, et al. Integrative gene expression profiling reveals that dysregulated triple microRNAs confer paclitaxel resistance in non-small cell lung cancer via co-targeting MAPT. Cancer Manag Res. 2019;11:7391–404.
Mokhlesi A, Talkhabi M. Comprehensive transcriptomic analysis identifies novel regulators of lung adenocarcinoma. J Cell Commun Signal. 2020;14(4):453–65.
Khomenko TM, Zakharenko AL, Chepanova AA, et al. Promising new inhibitors of Tyrosyl-DNA phosphodiesterase I (Tdp 1) combining 4-arylcoumarin and monoterpenoid moieties as components of complex antitumor therapy. Int J Mol Sci. 2019;21(1):126.
Rosell R, Moran T, Queralt C, et al. Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med. 2009;361(10):958–67.
Lynch TJ, Bell DW, Sordella R, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350(21):2129–39.
Agca CA, Kirici M, Nedzvetsky VS, Gundogdu R, Tykhomyrov AA. The effect of TIGAR knockdown on apoptotic and epithelial-mesenchymal markers expression in doxorubicin-resistant non-small cell lung cancer A549 cell lines. Chem Biodivers. 2020;17(9):e2000441.
Manabe S, Kasajima R, Murakami S, et al. Analysis of targeted somatic mutations in pleomorphic carcinoma of the lung using next-generation sequencing technique. Thoracic Cancer. 2020;11(8):2262–9.
Yang W, You N, Jia M, et al. Undetectable circulating tumor DNA levels correlate with low risk of recurrence/metastasis in postoperative pathologic stage I lung adenocarcinoma patients. Lung Cancer. 2020;146:327–34.
Rosell R, Bivona TG, Karachaliou N. Genetics and biomarkers in personalisation of lung cancer treatment. Lancet. 2013;382(9893):720–31.
Chen JA, Riess JW. Optimal management of patients with advanced NSCLC harboring high PD-L1 expression and driver mutations. Curr Treat Options Oncol. 2020;21(7):60.
Peters S, Camidge DR, Shaw AT, et al. Alectinib versus crizotinib in untreated ALK-positive non-small-cell lung cancer. N Engl J Med. 2017;377(9):829–38.
Verma P, Ghosh A, Ray M, Sarkar S. Lauric acid modulates cancer-associated microRNA expression and inhibits the growth of the cancer cell. Anticancer Agents Med Chem. 2020;20(7):834–44.
Kirkland JB. Niacin requirements for genomic stability. Mutat Res. 2012;733(1–2):14–20.
Setia MS. Methodology series module 5: sampling strategies. Indian J Dermatol. 2016;61(5):505–9.
Wang C, Li S, Liu J, et al. Silencing of S-phase kinase-associated protein 2 enhances radiosensitivity of esophageal cancer cells through inhibition of PI3K/AKT signaling pathway. Genomics. 2020;112(5):3504–10.
Ueda K, Nakahara T, Akanuma K, Mori A, Sakamoto K, Ishii K. Differential effects of LY294002 and wortmannin on neurons and vascular endothelial cells in the rat retina. Pharmacol Rep. 2013;65(4):854–62.
Yang P, Zhao J, Hou L, Yang L, Wu K, Zhang L. Vitamin E succinate induces apoptosis via the PI3K/AKT signaling pathways in EC109 esophageal cancer cells. Mol Med Rep. 2016;14(2):1531–7.
Li C, Liu DR, Li GG, et al. CD97 promotes gastric cancer cell proliferation and invasion through exosome-mediated MAPK signaling pathway. World J Gastroenterol. 2015;21(20):6215–28.
Acknowledgements
Not applicable.
Funding
This study was financially supported by the Startup fund from the Southern Medical University [grant No. G820282016], the Natural Science Foundation Council of China [grant No. 31501080, 32070676], Natural Science Foundation of Guangdong Province [grant No. 2021A1515010737], Hong Kong Baptist University Strategic Development Fund [grant No. SDF13-1209-P01, SDF15-0324-P02(b) and SDF19-0402-P02], Hong Kong Baptist University Interdisciplinary Research Matching Scheme [grant No. RC/IRCs/17–18/04].
Author information
Authors and Affiliations
Contributions
GXW, MBH, and DGG provided the research concept and designed the study. JQC, YPC, and KXW conducted the analyses and wrote the manuscript. YL, JW, and WM participated in data analysis. HLY, QPL, QW and HDW conducted experiments. APL, MBH and DGG contributed to revising and proof-reading the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Human lung cancer A549 cells were obtained from GuangZhou Jennio Biotech Co., Ltd. The ethics committee of Southern Medical University confirms that this study would have had the need for ethics approval waived.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supporting Information.
Additional file 2: Additional Table 1.
All herbal components of SMD. Additional Table 2. Active components of SMD. Additional Table 3. Predicted targets of active components from SMD. Additional Table 4. Pathogenic genes of lung cancer downloaded from DisGeNET database. Additional Table 5. The CDR of active components.
Additional file 3: Additional Figure 1.
Construct complex components-targets-pathogenic genes-disease (C-T-P-D) network. Green units represent active components of SMD, blue units represent predicted targets of active components and red units represent predicted pathogenic genes of lung cancer. The gray lines indicate the interactions. Additional Figure 2. Full distribution of KFC targets on merged paths. The red units denote the KFC targeted cross-talk genes shared by multiple pathways, and the red dashed line connects them together in different pathways. The blue units indicate that the KFC targeted genes exist only in one pathway. The white units are annotations or nontargeted proteins.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cai, J., Chen, Y., Wang, K. et al. Decoding the key compounds and mechanism of Shashen Maidong decoction in the treatment of lung cancer. BMC Complement Med Ther 23, 158 (2023). https://doi.org/10.1186/s12906-023-03985-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-023-03985-y